*N60,000, Every Six Months
*Bill Clinton, WHO Speak On New Drug
*Countries With Rising Infection Rates Won’t Benefit
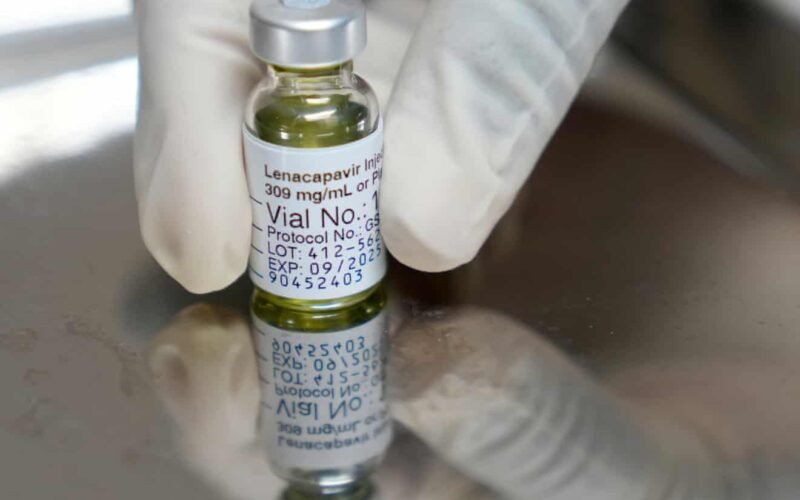
Cheap supplies of a groundbreaking twice-yearly HIV prevention jab will be available in many poorer countries within two years, funders have promised.
The drug, Lenacapavir, will cost $40 (about N60,000) a patient a year in 120 low- and middle-income countries (LMICs) from 2027, under two agreements with generic drug manufacturers announced this week.
Last year there were 1.3m new HIV infections globally and experts have said that Lenacapavir, as a preventive drug or “pre-exposure prophylaxis” (PrEP), could have a transformative effect on that figure.
The drug, given as an injection every six months, almost completely prevented new cases of HIV in clinical trials.
Official data show that as of 2021, there were approximately 1.9 million people living with HIV in Nigeria with almost 1.7 million on antiretroviral treatment, as well as an estimated 74,000 new HIV infections same year, a significant slash from about 120,000 in 2010.
World Health Organization (WHO) recommended it as a preventive drug in July, with the Director General (DG), Dr Tedros Adhanom Ghebreyesus, describing it as “the next best thing” to an HIV vaccine.
There had been questions about whether the drug would be affordable enough to make a difference in the countries with the highest rates of HIV. It was launched in the US with a list price of $28,218 a year.
Gilead Sciences, a biopharmaceutical company that develops medicines for unmet medical needs, particularly in virology (HIV/AIDS, hepatitis, COVID-19) and oncology, which brought the drug to market, has now granted voluntary licences to six generic manufacturers, including Dr Reddy’s and Hetero Labs, to supply the product in the 120 LMICs through national HIV programmes and organisations such as the Global Fund.
The 120 countries are many in Sub-Saharan Africa and Southeast Asia with high HIV incidence rates.
Unitaid, the Clinton Health Access Initiative (Chai) and the Johannesburg-based Wits RHI have entered into partnership with Dr Reddy’s Laboratories, while the Gates Foundation has an agreement with Hetero Labs.
The $40 price tag will put the injectable drug in the same bracket as HIV-prevention pills, which many people at higher risk of infection struggle to take.
The stigma surrounding HIV often means they want, or need, to hide the fact they are taking them.
Unitaid’s director, Dr Philippe Duneton, said: “Securing a $40 price for the twice-yearly Lenacapavir injection for PrEP is a historic breakthrough that proves the most advanced tools can be made affordable from the very start.”
Antiretroviral drugs to treat HIV were not available in sub-Saharan Africa for about a decade after they became an option for people living with HIV in high-income countries, resulting in millions of deaths.
Bill Clinton, the former US president who co-founded Chai, said Lenacapavir’s rollout represented “a genuine chance to end” the global epidemic of HIV.
Beatriz Grinsztejn, president of the International AIDS Society, said: “We welcome Lenacapavir generics being made affordable – a vital step to expand access – but availability in 2027 still feels far away.”
“With the HIV response in a funding crisis, countries are already making difficult trade-offs,” she said. “To realise the full potential of this innovation, PrEP options like Lenacapavir must reach the most vulnerable people, which requires urgent, additional investment to avoid delays or denied access.”
There have been efforts to increase access in the period before generics become available, with Pepfar, the Global Fund and the Children’s Investment Fund Foundation promising funding to procure preventive Lenacapavir for LMICs. Gilead has said it will provide them with the drug at no profit.
However, the Trump administration has suggested its funding should only apply to Lenacapavir for pregnant and breastfeeding women, which would exclude other high-risk groups such as men who have sex with men, sex workers, people who use drugs and prisoners.
Furthermore, many countries with growing numbers of HIV cases are not on the list of 120 “high-incidence, resource-limited countries” that was agreed with Gilead.
Unitaid said it “remains committed to addressing access barriers in countries not covered by the existing agreements”.
PHOTO CAPTION: The HIV prevention injectable drug.